Neurotrophic Keratitis: Protecting Your Vision
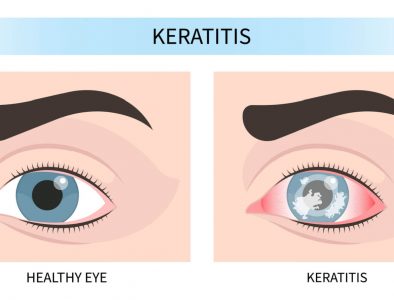
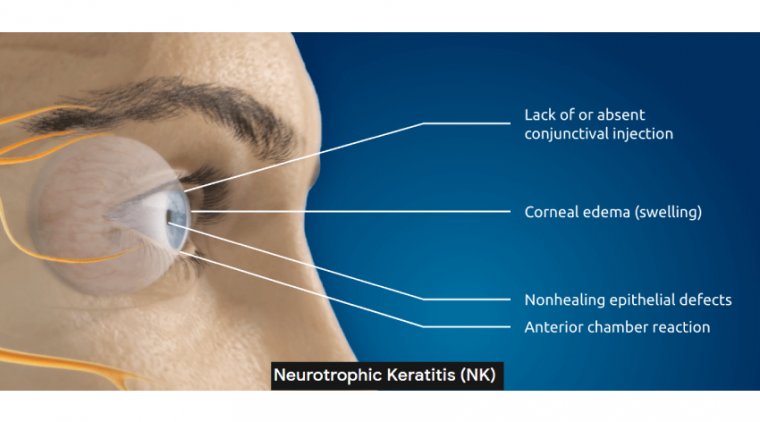
Neurotrophic Keratitis (NK) is a rare, progressive eye disease caused by damage to the corneal nerves. These nerves normally act as an early-warning system, triggering blinking, tearing, and repair responses when the cornea is injured. When they stop working properly, the cornea loses its ability to heal, leading to persistent defects, ulcers, scarring, and—if left untreated—vision loss.
NK is considered an orphan disease, affecting fewer than 5 in 10,000 people. Because it often develops silently, many patients don’t know they have NK until it reaches advanced stages.

What Causes NK?
NK is not a stand-alone disease but usually develops as a complication of other conditions, including:
- Herpes eye infections (Herpes Simplex & Herpes Zoster): Viruses can permanently damage corneal nerves.
- Eye surgery or trauma: Procedures like LASIK, corneal transplants, or even cataract surgery sometimes disrupt nerve function.
- Contact lens overuse: Long-term or improper lens wear can reduce corneal sensitivity and healing capacity.
- Systemic diseases: Diabetes and multiple sclerosis are linked to NK because they damage nerves throughout the body, including the eyes.
- Other causes: Rare genetic conditions or tumors pressing on the trigeminal nerve can also lead to NK.
Why NK is Hard to Treat
Unlike many eye conditions, NK doesn’t just affect the surface of the cornea—it undermines the cornea’s ability to heal itself. Standard therapies (like lubricating drops) only relieve symptoms but don’t fix the underlying nerve damage. This is why advanced therapies focus on regenerating or bypassing the damaged nerves, a much harder task than treating inflammation or infection.
How NK is Diagnosed
Early NK can be difficult to spot, because patients often don’t feel pain when their cornea is damaged. That’s why diagnosis requires an eye specialist.
Who to see: Usually an ophthalmologist (a medical doctor specializing in eye diseases) diagnoses and manages NK. Optometrists may detect early warning signs and refer patients.
Tests used: Doctors measure corneal sensitivity with specialized tools and use high-resolution microscopes to look for ulcers, thinning, or delayed healing. Fluorescein dye may also be used to highlight damaged areas.
Who is at Risk?
Age: NK can occur at any age but is more common in adults over 50.
Health conditions: People with diabetes, multiple sclerosis, or a history of shingles are at higher risk.
Genetics: Rare hereditary conditions that affect nerve function may also play a role.
Eye surgery patients: Those who have undergone corneal or refractive surgeries may have reduced corneal sensitivity.
Treatment Options
- Mild: Artificial tears, protective drops, or special contact lenses.
- Moderate: Serum eye drops or amniotic membrane grafts.
- Severe: Procedures like partial eyelid closure, corneal transplants, or new therapies that help regenerate nerves.
Why Early Detection Matters
NK often develops silently, with few or no symptoms. Regular eye exams are crucial if you’ve had eye surgery, infections, or other risk factors.
Protecting Your Vision
- Get yearly eye exams—even if your eyes feel fine.
- Report sudden vision changes right away.
- Follow your doctor’s care plan to protect your eyes.
How You Can Get Involved
At Ora, we’re committed to developing innovative solutions for every eye condition. If you or a loved one has NK and would like to learn more about clinical trial opportunities, contact our call center at 1-866-393-3767 (1-866-EYE-DROP) or email orarecruiting@oraclinical.com.